Transcription
Emerg Med Clin N Am25 177–188Hyperbaric Oxygen Therapyin the Treatment of OpenFractures and Crush InjuriesMark F. Buettner, DO, ABEM*,Derek Wolkenhauer, RRT, CHTGreat River Wound and Hyperbaric Clinic, Center for Rehabilitation,1401 West Agency Road, West Burlington, IA 52655, USATraumatic injuries to the extremities that involve tissue ischemia areknown to share a common dynamic pathophysiology. In the practice of hyperbaric medicine such injuries fall within a group known as the acute traumatic peripheral ischemias (ATPIs). These injuries include open fracturesand crush injuries, skeletal muscle compartment syndromes, thermal burns,frost bite and threatened flaps, and grafts and replantations. In their variousforms, these injuries share a common pathophysiology involving (1) a triadof tissue ischemia, hypoxia, and edema, (2) a gradient of tissue injury, and(3) a capacity for the injury to become self perpetuating. Early administration of hyperbaric oxygen therapy (HBOt) is reported to be beneficial whenprovided as an adjunct to appropriate surgical interventions for the ATPIs.Emergency department management of these injuries is part of the core curriculum of emergency medicine residency training. Emergency physiciansshould familiarize themselves with this treatment modality because of theirrole in the early management of these injuries. The focus of this article is onthe use of HBOt in the treatment of open fractures and crush injuries.BackgroundHyperbaric oxygen is a therapy in which a patient breathes 100% oxygenwhile inside a treatment chamber at a pressure greater than that of sea level.The earliest cited application of treating patients under pressure dates backto 1662 when the British clergyman Henshaw [1] constructed a sealed* Corresponding author.E-mail address: (M.F. Buettner).0733-8627/07/ - see front matter Ó Elsevier Inc.
178BUETTNER & WOLKENHAUERchamber he called a ‘‘domicilium.’’ By connecting his vessel to valved organbellows, he was able to increase or decrease the air pressure within. Withoutany scientific basis he treated a variety of acute and chronic illnesses. In thenineteenth century discoveries were made allowing safer and more effectivedelivery of anesthesia within a compressed air environment. Decompressionsickness was first identified among bridge caisson workers in the 1850s.Compression therapy for this disorder was first provided in 1889. Modern-day use of hyperbaric oxygen therapy emerged in 1955 with the workof Churchill-Davidson [2]. The high-oxygen environment was used to potentiate the effects of radiation therapy in cancer patients. That same year, theDutch surgeon Ite Boerema [3] proposed using HBOt to enhance toleranceto circulatory arrest during cardiac surgery. The promising results of his animal studies led to the construction of a large hyperbaric operating chamberat the University of Amsterdam. Boerema [3] performed a variety of surgeries within this chamber for conditions such as transposition of the great vessels, tetralogy of Fallot, and pulmonic stenosis. His first publicationappeared in 1956. In the early 1960s the first reports on the positive effectsof HBOt for anaerobic infections and carbon monoxide poisonings werepublished [4,5]. The 1970s witnessed both degradation and decline in thefield. On the heels of the discoveries found in the 1960s researchers eagerlysought other applications for HBOt. Experiments were performed using it ina variety of debilitating conditions. Positive reports were largely anecdotal,touting the ‘‘good results’’ without regard for scientific methodology [6]. Indiscriminate use of HBOt led to the need for regulation. There were no formal guidelines for insurers to reference regarding payment for the valid useof HBOt. In 1976, the Undersea Medical Society formed an ad hoc committee to work with Medicare and Blue Cross. As a result, the first edition ofthe Hyperbaric Oxygen Therapy Committee Report was published. Formalindications for the valid use of HBOt were established based on scientificmerit. With periodic revisions, the committee report remains the authorityon approved indications for HBOt within the United States (Fig. 1).PhysiologyThe primary means for oxygen transport is in the form of oxyhemoglobinbound within the erythrocyte. At sea level the barometric pressure is 1 atmosphere absolute (ata). At 1 ata the partial pressure of alveolar oxygen (PAO2)is about 100 mm Hg. Also at 1 ata hemoglobin is about 97% oxygen saturated (SaO2 ¼ 97) and yields an oxygen content (HbO2 þ plasma dissolvedO2) of about 19.8 mL oxygen per dL blood. Under pressure, as the PAO2 reaches 200 mm Hg, hemoglobin becomes fully saturated with oxygen (SaO2 ¼100%). Further increases in pressure beyond a PAO2 of 200 mm Hg will notresult in an increase in oxyhemoglobin. Therefore, the superoxygenatedstate achieved in a hyperbaric oxygen environment is attributed to theamount of oxygen physically dissolved in the plasma. When air is breathed
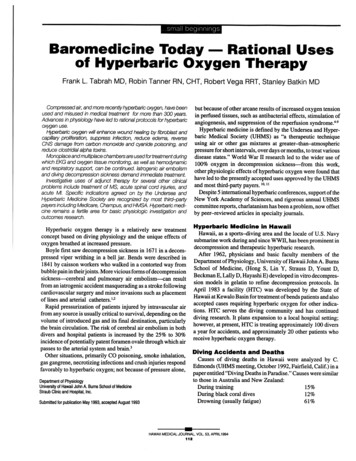
HYPERBARIC OXYGEN THERAPY179Fig. 1. Monoplace hyperbaric oxygen chamber at Great River Wound and Hyperbaric ClinicWest Burlington, Iowa. (Courtesy of Perry Baromedical, Riviera Beach, FL; with permission.)at sea level (1 ata), only 1.5% of the oxygen content is related to oxygen dissolved in plasma. Comparatively, when 100% oxygen is breathed at a pressure of 3 ata, a PAO2 of 2200 mm Hg is generated, dissolving another 6.8 mLof oxygen into each dL of blood, resulting in an arterial oxygen tension(PaO2) of about mm Hg (Fig. 2). A healthy adult at rest uses about6 mL of oxygen per dL of circulating blood. Therefore, as demonstratedin Boerema’s 1960 study ‘‘Life Without Blood’’ [7], life can be sustainedwithout the need for erythrocytes while in a hyperbaric oxygen environmentat a pressure of 3 ata.Crush injury pathophysiologyIf the amount of energy transfer during a crush injury is sufficient, a gradient of tissue injury expands from the impact site (Fig. 3). The most immediate injury is the primary zone of tissue destruction. This region ofFig. 2. Combined blood oxygen content bound to hemoglobin and dissolved in plasma at highlevels of blood PO2. (From Sheffield PJ, Smith PS. Physiologic and pharmacological basis ofhyperbaric oxygen therapy. In: Bakker DJ, Cramer FS, editors. Hyperbaric surgery perioperative care. Flagstaff (AZ): Best Publishing Company;. p. 68; with permission.)
180BUETTNER & WOLKENHAUERFig. 3. Zones of injured tissues relative to the crush impact and the secondary perpetuation ofinjury.injured tissue may be rendered nonviable regardless of intervention. Thenext zone along the gradient of injury is composed of variably injuredor variably ischemic tissues. Most therapeutic interventions are targetedwithin this penumbra of tissues. The outermost zone along the gradientof injury is composed of minimally injured to noninjured tissues. A selfperpetuating secondary injury may occur to tissues at any point alongthe injury gradient.Secondary injuryIschemiaA decrease in blood perfusion to the variably injured tissues is the initialevent leading to secondary injury. Ischemia may result from direct traumaticinjury to blood vessels. Ischemia also may arise indirectly. The indirectmechanism for ischemia often is multifactorial and may include one ormore of the following: fluid leakage (edema, hemorrhage) with or withoutvascular collapse from the external pressure of the tissue fluid (compartmentsyndrome); vasoconstriction; stasis; occlusion. The indirect mechanisms forischemia within the microcirculation are the largest contributor to the secondary injury.
HYPERBARIC OXYGEN THERAPY181HypoxiaCellular processes involved in wound repair are heavily oxygen dependant. The zone of variably injured tissues has an increased oxygen demandat a time of diminished perfusion. Oxygen demands may increase by a factorof greater than 20 [8]. Wound-repair mechanisms such as fibroblast activityand collagen formation are compromised under hypoxic conditions [9]. Anincreased risk of infection develops with the failure of oxygen-dependanthost immune functions. Hypoxic cells cannot retain intracellular water,leading to cytogenic edema.EdemaEdema is a profound contributor to tissue hypoxia. When fluid accumulates within the extracellular space, the distance from the capillary wall tothe injured cell is greater. Therefore, less oxygen reaches the injured cellto exert repair. Vasodilatation of the proximal arterial vasculature increasesblood flow to the site of injury. This reflex results in vasogenic edema. Whencombined with increased bleeding from the injured vessels, fluid accumulates in the interstitial space. Collapse of the capillary bed occurs as thepressure within the interstitial space exceeds capillary filling pressures(12–32 mm Hg). Cellular hypoxia is propagated.Reperfusion injuryReperfusion contributes to the perpetuation of the secondary injury.Neutrophils adhere to postcapillary venules after a period of ischemia andduring reperfusion. This process results in a release of toxic oxygen free radicals. Oxygen free radicals are destructive to tissues in several ways: the induction of a no-reflow phenomenon by the vasoconstriction of precapillaryarterioles, lipid peroxidation of cell membranes, and the formation of peroxynitrite when the oxygen free radicals react with endothelial-generated nitricoxide.The net result is a self-perpetuating secondary injury. If left unchecked,this secondary injury may result in a volume of tissue necrosis much largerthan and remote from the primary zone of tissue destruction. When the drugoxygen is delivered within a hyperbaric environment, its pharmacodynamicsmitigates the pathophysiology of ischemia.Pharmacodynamics of hyperbaric oxygen therapyDiffusion radiusTo exert its effects, oxygen must travel out of the arterial end of the capillary wall through the interstitial space to the injured cell. This diffusion
182BUETTNER & WOLKENHAUERradius of oxygen from the arterial end of the capillary into the interstitialspace has been calculated to traverse a distance of 64 mm. With HBOt at3 ata, this diffusion radius has been calculated to traverse a distance of247 mm (Fig. 4) [10]. During the immediate postinjury period of a crush injury the maintenance of tissue oxygenation is critical [11].Vascular responseOxygen breathing results in smooth muscle contraction of the arterialvasculature resulting in up to a 20% reduction of blood flow to the limb[12]. This response is physiologic, and it is observed in healthy tissues.With an increase in upstream arterial resistance comes a drop in downstream capillary hydrostatic pressure. The drop in local capillary hydrostaticpressure creates an environment that favors absorption. The increase in oxygen dissolved in plasma compensates for the reduction in blood flow. Conversely, Hammerlund and colleagues [13,14] have shown that with oxygenbreathing blood flow increases within the local microvasculature of bothacute and chronic wounds. The net response to HBOt within the variablyinjured tissues is a redistribution of perfusion and physiologic resorptionof edema.Cellular functionCellular function is restored when HBOt corrects the PO2 to normal orslightly elevated values. This restoration is manifested by enhancedFig. 4. Krogh-Erlang oxygen diffusion model used to estimate oxygen diffusion from the capillaries to surrounding tissue and the potential increase in oxygen diffusion distances with hyperbaric oxygenation. ATA, atmosphere absolute; R, radius. (From Sheffield PJ, Smith PS.Physiologic and pharmacological basis of hyperbaric oxygen therapy. In: Bakker DJ, CramerFS, editors. Hyperbaric surgery perioperative care. Flagstaff (AZ): Best Publishing Company; p. 68; with permission.)
HYPERBARIC OXYGEN THERAPY183epithelialization, fibroplasia, collagen synthesis, angiogenesis, and leukocytebactericidal-killing mechanisms [15,16]. The enhanced fibroblast activity canlast up to 72 hours following a hyperbaric oxygen exposure. HBOt reducesthe secondary injury by blunting the release of oxygen free radicals. Morespecifically, the Beta2 integrin system is disrupted, preventing neutrophil adherence to the postcapillary venules [17]. Hyperbaric oxygen also antagonizes lipid peroxidation of the cell membrane [18]. Erythrocyte sludging isreduced because of enhanced erythrocyte deformability in response toHBOt (Fig. 5) [19].Fig. 5. Hyperbaric oxygen mediates the effects of crush injuries primarily through four mechanisms. These mechanisms also are useful adjuncts in managing the injuries in the other acutetraumatic peripheral ischemias. HBO, hyperbaric oxygen. (From Strauss B. Crush injury, compartment syndrome and other acute traumatic peripheral ischemias. In: Kindwall E, Whalen H,editors. Hyperbaric medicine practice. 2nd (revised) edition. Flagstaff (AZ): Best PublishingCompany;. p. 760; with permission.
184BUETTNER & WOLKENHAUERClinical applicationDespite all that is understood about the physiologic and pharmacodynamic properties of hyperbaric oxygen, guidelines for its clinical applicationin the treatment of the ATPIs as a group are limited. The lack of guidelinesis related to a noticeable paucity of randomized clinical trials in the literature. The vast majority of the clinical literature is in the form of case reports.A well-designed clinical trial allows comparison between treatment groupsso that it is possible to identify which patients actually need the therapyto heal and which ones do not. Clinical guidelines are derived more accurately from such studies. Unfortunately, the complex and variable natureof these injuries as a group makes it difficult to develop well-designed clinicaltrials.The clinical recommendations for the use of HBOt in open fractures andcrush injuries are perhaps the best founded. In 1979 Strauss [20] had summarized more than 700 positive case reports in the use of HBOt